Overweight and obesity are the plague of the 21st century, spreading wider and wider. According to research conducted in Poland in 2014, they have already been diagnosed in 62% of adult men and 46% of women. Excessive body weight is a result of inadequate energy intake compared to insufficient energy expenditure. Unfortunately, easy access to highly processed food with high sugar content, coupled with low fiber intake and very low physical activity, paves the way to obesity and, consequently, to metabolic diseases such as insulin resistance, diabetes, coronary heart disease, and hypertension. How can we protect ourselves from overweight? It turns out that taking care of the composition of gut microbiota is an effective way.
Overweight and obesity are the plague of the 21st century, spreading wider and wider. According to research conducted in Poland in 2014, they have already been diagnosed in 62% of adult men and 46% of women. Excessive body weight is a result of inadequate energy intake compared to insufficient energy expenditure. Unfortunately, easy access to highly processed food with high sugar content, coupled with low fiber intake and very low physical activity, paves the way to obesity and, consequently, to metabolic diseases such as insulin resistance, diabetes, coronary heart disease, and hypertension. How can we protect ourselves from overweight? It turns out that taking care of the composition of gut microbiota is an effective way.
MICROFLORA – AN ADDITIONAL ORGAN IN THE HUMAN BODY
The large intestine is the end of the approximately 10-meter-long muscular digestive tract. It is home to various types of microorganisms: bacteria, fungi, and protozoa.
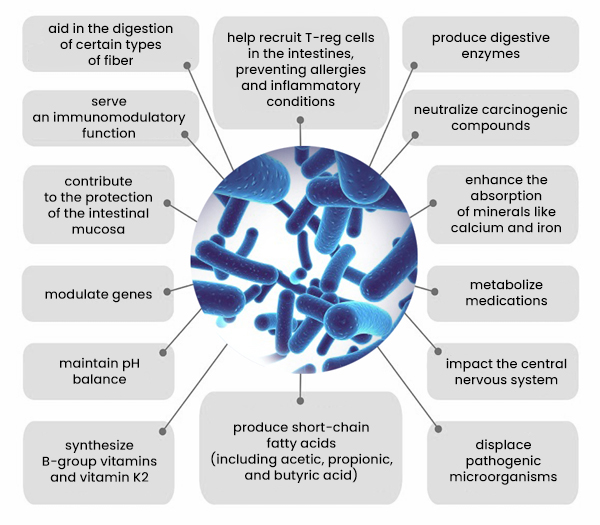
The bacterial gut flora contains about 100 times more genes than the human genome, weighs about 2 kg, and consists of over 100 trillion bacteria, making up 90% of all microorganisms living in the intestine. The microbiome plays such a crucial role in the functioning of the body that some scientists consider it to be a distinct organ.
The colonization of the intestine by bacteria begins during childbirth when a child passes through the mother’s birth canal. This way, the child’s gut gets mainly colonized by bacteria from the Lactobacillus genus (anaerobes tolerating oxygen). By the age of 3, each person’s unique microbiome is almost fully formed. The composition of bacterial flora depends on the host’s genotype, mode of birth (natural birth or cesarean section), age, geographical location, and dietary habits. In a balanced state, the colon is dominated by beneficial anaerobic bacteria, such as Bifidobacterium, Clostridium, Lactobacillus, Bacteroides, and Eubacterium.
DYSBIOSIS – A THREAT TO HEALTH
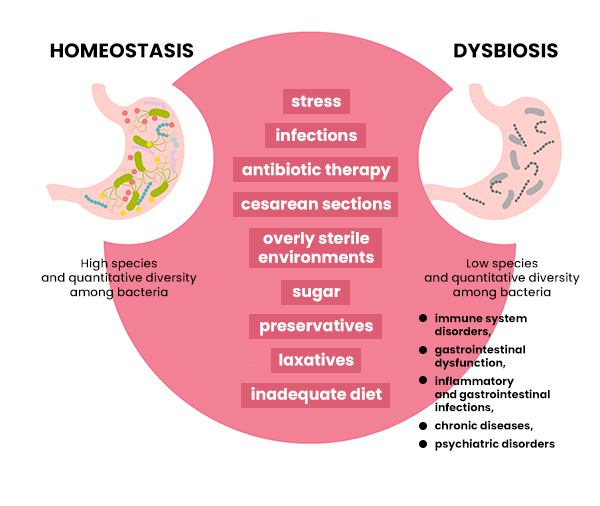
Unfortunately, nowadays, more and more people suffer from disruptions in gut flora. Its improper composition is the cause of dysbiosis, which, in turn, leads to many ailments and diseases. Factors contributing to this imbalance include stress, infections, antibiotic therapy, cesarean section, overly sterile lifestyles, and an inadequate diet filled with processed food, preservatives, and sugar.
These are the main causes of dysbiosis, which leads to a decrease in species and quantitative diversity among bacteria inhabiting the intestines. Dysbiosis, in turn, contributes to the development of local inflammation, leaky gut syndrome, allergies, autoimmune diseases, dysfunction of the immune, hormonal, and digestive systems, as well as abnormal lipid metabolism, which probably plays a significant role in the development of obesity.
The bacterial gut flora contains about 100 times more genes than the human genome, weighs about 2 kg, and consists of over 100 trillion bacteria, making up 90% of all microorganisms living in the intestine. The microbiome plays such a crucial role in the functioning of the body that some scientists consider it to be a distinct organ.
DIFFERENCES IN THE COMPOSITION OF GUT BACTERIAL FLORA IN LEAN AND OVERWEIGHT/OBESE INDIVIDUALS
With the growing problem of overweight and obesity, scientists have discovered certain relationships between excess weight and the gut bacterial flora of humans. It has been observed that the composition of gut flora in overweight or obese individuals differs significantly from that of lean individuals. Lean individuals have a higher number of Bacteroides bacteria (beneficial for health and promoting a lean body) and a higher ratio of their occurrence compared to Firmicutes bacteria (associated with increased risk of overweight, obesity, and allergic reactions). Moreover, the microbiome in lean individuals is more diverse than that of obese individuals, regardless of their place of residence. It should be noted that having a rich and diverse bacterial flora in the intestines promotes homeostasis or a state of balance. The fewer bacteria present, the more vulnerable we are to dysbiosis. Additionally, the gut flora of obese individuals is more often colonized by Escherichia coli bacteria (anaerobic bacteria that, under specific conditions, possess pathogenic properties) and Staphylococcus aureus (one of the more dangerous species of staphylococcus). Obese individuals also harbor more groups of bacteria that efficiently break down carbohydrates, which may contribute to weight gain.
It has been observed that the composition of gut flora in overweight or obese individuals differs significantly from that of lean individuals. Their microbiome is less diverse and contains fewer bacteria promoting a lean body, while having higher quantities of those that more efficiently break down carbohydrates.
GUT BACTERIA FEED ON WHAT YOU EAT – THE EFFECT OF DIET ON MICROFLORA COMPOSITION
Diet undoubtedly affects human health. It has been observed that gut microbiota can influence body weight, insulin sensitivity, and the metabolism of sugars and lipids. Thanks to the symbiosis of humans and gut bacteria, it is possible to obtain energy from compounds that are not broken down by digestive enzymes but rather by the gut flora. This way, we can obtain 80 to 200 kcal daily.
First and foremost, it is crucial to remember that what a person consumes becomes the nourishment for their gut bacteria. Different bacterial species prefer different nutrients. Hence, significant differences in the composition of gut flora are noted among individuals following drastically different diets. Studies have shown that a meat-rich diet affects the gut microbiota, which metabolizes it, leading to the production of harmful compounds associated with cardiovascular diseases. Individuals on a meat-based diet show an increase in Firmicutes (bacteria promoting weight gain) and Enterobacteriaceae (mostly non-pathogenic bacteria that can cause infections in immunocompromised individuals). Conversely, vegetarians have a predominance of Bacteroidetes in their gut microbiota. They also exhibit a simultaneous decrease in the number of Clostridium bacteria (some species are pathogenic, producing potent exotoxins, while others are opportunistic microorganisms) and a reduction in Firmicutes and Enterobacteriaceae. A diet rich in complex carbohydrates (fiber) that serve as nourishment for gut bacteria shapes a diverse bacterial flora, benefiting human health. Changes in gut microbiota composition have also been observed after following a reducing diet, resulting in a significant reduction in the number of Firmicutes bacteria along with an increase in Bacteroides.
What a person consumes becomes the nourishment for their gut bacteria. Different bacterial species prefer different nutrients. Hence, significant differences in the composition of gut flora are noted among individuals following drastically different diets.
CAN GUT BACTERIA AFFECT HUMAN APPETITE?
Gut microorganisms can send signals of satiety or hunger to the brain by increasing the level of leptin – the hormone responsible for feeling fullness – or by suppressing ghrelin, the hormone responsible for feeling hunger. Therefore, gut bacteria have a significant influence on human appetite.
BACTERIA AND INFLAMMATION AND EXCESSIVE WEIGHT GAIN
When gut bacteria do not receive proper nourishment, they fail to perform their functions. Consequently, the intestinal walls become permeable, allowing bacteria to enter the bloodstream, leading to inflammation. Bacterial substances can also attach to organ cells or adipose tissue, leading to fat accumulation.
PROBIOTICS – A FACTOR MODULATING MICROFLORA
Recently, the number of publications concerning the beneficial effects of probiotics on weight reduction has increased. By providing patients with specific probiotic strains, attempts are made to modify their gut flora composition to have a positive impact on maintaining optimal weight.
According to the World Health Organization, probiotics are live microorganisms that, when administered in appropriate amounts, provide health benefits to the host.
One study conducted in Russia in 2013 showed the influence of probiotic strains on the weight of the study subjects. The study found that a diet enriched with strains of Lactobacillus plantarum TENSIA and Lactobacillus gasseri SBT2055 led to a reduction in body weight, BMI, triglyceride levels, waist circumference, subcutaneous and visceral fat tissue in obese patients.
PREBIOTICS – NOURISHMENT FOR GOOD GUT BACTERIA
Prebiotics can also have a beneficial effect on some metabolic processes in obese individuals. According to the FAO/WHO, prebiotics are food ingredients that beneficially affect human health by influencing the bacteria in the large intestine. Each day, an adult should consume between 20 to 40 grams of fiber. Prebiotics include oligosaccharides such as fructooligosaccharides (FOS), galactooligosaccharides (GOS), isomaltooligosaccharides (IMO), xylooligosaccharides (XOS), lactulose, and soy oligosaccharides (SBOS). The group of polysaccharides includes pectins, guar gum, oat gum, and inulin. Inulin, which is a common prebiotic, can be found as a dietary supplement, but it also naturally occurs in many fruits and vegetables, particularly in onions, garlic, chicory, and Jerusalem artichokes. Resistant starches and whole grains are also rich in nutrients that serve as nourishment for beneficial gut bacteria. Almost all complex plant carbohydrates and plant fiber can be considered prebiotics.
Studies have shown that the intake of 12 grams of inulin per month reduces VLDL fraction (triglyceride levels) in the blood by 27% and cholesterol by 5%. It is also presumed that oligofructose accelerates lipid catabolism (fat breakdown). Studies on animals have also noted that the administration of prebiotics significantly reduced cancerogenesis rates.
Results from a 2015 study evaluating the impact of prebiotic consumption on the body weight of women showed an increase in the number of Bifidobacterium longum, Bifidobacterium pseudocatenulatum, and Bifidobacterium adolescentis in the group consuming inulin compared to the placebo group. The subjects also showed improved glucose tolerance and reduced insulin resistance. Studies also note the positive impact of using synbiotics (probiotics administered in combination with prebiotics) on weight reduction.
Until now, research has provided ample evidence of the enormous importance of the microbiota for human health. Having a rich and diverse bacterial flora is undoubtedly the most beneficial. We can achieve this by leading an active lifestyle and consuming a diet rich in vegetables, which are a source of prebiotics, as well as fermented foods containing live bacteria cultures – the best probiotics (such as sauerkraut, pickled cucumbers, fermented dairy products, or apple cider vinegar). However, it is essential to remember that when fermented foods undergo further processing, such as pasteurization, baking, or filtering, the probiotic bacteria are destroyed.
Źródło:
Justyna Brzezińska – SKŁAD FLORY JELITOWEJ A ROZWÓJ NADWAGI I OTYŁOŚCI – czy mają ze sobą coś wspólnego? Diet.Point, nr 2(3)/2019 , str. 4-8
Bibliography:
1.Davidson J., The psychobiotics revolutions, Psychology Today, Natures bounty, 2014
2.Domingues-Bello M.G. Costello E.K. Contreras M. Magris M. Hidalgo G. Fierer N. Knight R., Delivery Mode Shapes the Acquisition and Structure of the Initial Microbiota across Multiple Body Habitats in 3.Newborns, Proc. Natl. Acad. Sci. USA, 107 (26), 2010, s. 11971-11975
4.Dziewiatowska J. Janczy A. Steinka I. Pieszko M. Małgorzewicz S., Związek pomiędzy mikroflorą jelitową a otyłością, Forum Zaburzeń Metabolicznych 2014, tom 5, nr 1, 20–25
5.Enders G. Historia wewnętrzna, wyd. 2014
6.Fujimura K.E. Slusher N.A. Cabana M.D. Lynch S.V., Role of the gut microbiota in defining human health, Expert Rev Anti Infect Ther. 2010 Apr; 8(4): 435–454.
7.Guarner F., Khan G.A., Garisch J, Eliakim R., Gangl A., Thomson A., Krabshuis J., Lemair T., Probiotics and prebiotics, World Gastroenterology Organisation Global Guidelines, October 2011, 28
8.Jarosz M., Normy żywienia dla populacji polskiej – nowelizacja, Instytut Żywności i Żywienia, 2012
9.Koeth R.A. Wang Z. Levison B.S. Buffa J.A. Org E. Sheehy B.T. Britt E.B. Fu X. Wu Y. Li L. Smith J.D. DiDonato J.A. Chen J. Li H. Wu G.D. Lewis J.D. Warrier M. Brown J.M. Krauss R.M. Tang W.W.H. Bushman F.D. 10.Lusis A.J. Hazen S.L., Intestinal Microbiota Metabolism of L-Carnitine, a Nutrient in Red Meat, Promotes Atherosclerosis, Nat. Med. 19 (5), 2013, s. 576-585
11.Mojka K., Probiotyki, prebiotyki i synbiotyki – charakterystyka i funkcje, Probl Hig Epidemiol 2014, 95(3): 541-549
12.Smith P.M. Howitt M.R. Panikov N. Michaud M. Gallini C.A. Bohlooly-Y M. Glikman J.N. Garret W.S., The Microbial Metabolites, Short-chain fatty acids, regulate colonic Treg homeostasis, „Science” 341, 2013, s. 569-573
13.Sonnenberg J. Sonnenberg E. Zdrowie zaczyna się w brzuchu, wyd 2015
14.Stachowicz N. Kiersztan A., Rola mikroflory jelitowej w patogenezie otyłości i cukrzycy, Postepy Hig Med Dosw (online), 2013; tom 67: 288-303
15.Śliżewska K. Nowak A. Barczyńska R. Libudzisz Z., Prebiotyki – Definicja, Właściwości i Zastosowanie w Przemyśle, Żywność. Nauka. Technologia. Jakość, 2013, 1 (86), 5-20
16.Ostrowska L. Smarkusz J., Modyfikacja mikroflory jelitowej sposobem zapobiegania lub leczenia otyłości i schorzeń metabolicznych? Forum Zaburzeń Metabolicznych 2016, tom 7, nr 2, 53–61